Billing For Services Not Provided To Medicare ?
Medicare Not-covered Services
At that place are two main categories of services which a physician may not be paid by Medicare:
- Services non deemed medically reasonable and necessary
- Not-covered services
In some instances, Medicare rules let a doc to bill the patient for services in these categories. Understanding these rules and how to use them in your practice increases the likelihood of getting paid for the services your patients need, even if Medicare doesn't comprehend them.
Other categories of services Medicare does not pay include bundled services and services for which another entity, such as workers' bounty, are primarily responsible (oftentimes referred to as "coordination of benefits").
Medically Reasonable and Necessary
A patient may ask for a service that Medicare does not consider medically reasonable and necessary nether the circumstances. For example, the patient wants the service more than frequently than Medicare allows or for a diagnosis that Medicare does non cover. Y'all can often verify coverage information by researching the service on the payer's website. If the patient's policy coverage is unclear, inform the patient that it may consequence in an out-of-pocket expense before performing the service.
At that place are two resources to help you determine if Medicare considers services to exist medically reasonable and necessary: national coverage determinations (NCDs) and local coverage determinations (LCDs). These documents provide information regarding CPT and Healthcare Common Procedure Coding System (HCPCS) codes, ICD-10 codes, billing information, as well as service delivery requirements.
The Centers for Medicare & Medicaid Services (CMS) offers an online, searchable Medicare Coverage Database that allows anyone to freely search NCDs, LCDs, and other Medicare coverage documents. The database has quick and avant-garde search capabilities to search by geography, Medicare contractor, key words, CPT codes, HCPCS codes, and ICD-10 codes.
Commercial insurance companies and some Medicaid payers will take similar types of information well-nigh their coverage guidelines on their websites. Stay up-to-date on these policies for your local payers to ensure claims are processed as medically reasonable and necessary.
Inform Patient of Potential Financial Responsibility
In all cases, if the patient's policy coverage is unclear, inform the patient that they may be responsible for paying for the service. This should be done before you provide the service.
If a Medicare patient wishes to receive services that may not be considered medically reasonable and necessary, or you feel Medicare may deny the service for another reason, you should obtain the patient's signature on an Advance Beneficiary Discover (ABN). Medicare requires an ABN be signed by the patient prior to first the procedure before you can beak the patient for a service Medicare denies as investigational or not medically necessary. Otherwise, Medicare assumes the patient did not know and prohibits the patient from being liable for the service.
You must explicate the ABN to the patient and the patient must sign it before the service is provided. The ABN must accept the following three components:
- Detailed description of the service to be provided;
- Estimated cost within $100; and
- Reason it is believed Medicare will not cover the service.
If an ABN is obtained, attach modifier -GA (waiver of liability argument issued as required by payer policy, individual case) to the line item(s) within the claim to indicate the patient has been notified.
The CMS website has boosted information and downloadable ABNs in several formats.
Non-covered Services
Certain services are never considered for payment past Medicare. These include preventive examinations represented past CPT codes 99381-99397. Medicare only covers three immunizations (flu, pneumonia, and hepatitis B) equally prophylactic physician services.
Cosmetic procedures are never covered unless there is a medically-necessary reason for a procedure. In this instance, you should certificate and lawmaking information technology equally such. Services rendered to immediate relatives and members of the household are not eligible for payment.
Non-covered services do non require an ABN since the services are never covered under Medicare. While not required, the ABN provides an opportunity to communicate with the patient that Medicare does non cover the service and the patient volition be responsible for paying for the service. Pre-emptive advice through a voluntary ABN can forestall negative patient perceptions of your exercise and facilitate collections. These modifiers are non required by Medicare, but do permit for clean claims processing and billing to the patient. There are three modifiers to consider when dealing with non-covered services:
- -GX– Discover of liability issued, voluntary payer policy. A -GX modifier should be attached to the line item that is considered an excluded, non-covered service. The -GX modifier indicates you provided the notice to the casher that the service was voluntary and likely not a covered service.
- -GY – Item or service statutorily excluded, does not meet the definition of any Medicare do good or for non-Medicare insurers, and is not a contract benefit. If you do non provide the casher with notice that the services are excluded from coverage, you should append modifier -GY to the line item. Modifier -GY indicates a notice of liability (ABN) was not provided to the beneficiary.
- -GZ – Detail or service expected to be denied as not reasonable and necessary. Modifier -GZ should exist added to the claim line when information technology is determined an ABN should have been obtained, but was not.
Utilizing ABNs and corresponding modifiers appropriately assists with compliance reporting in your function.
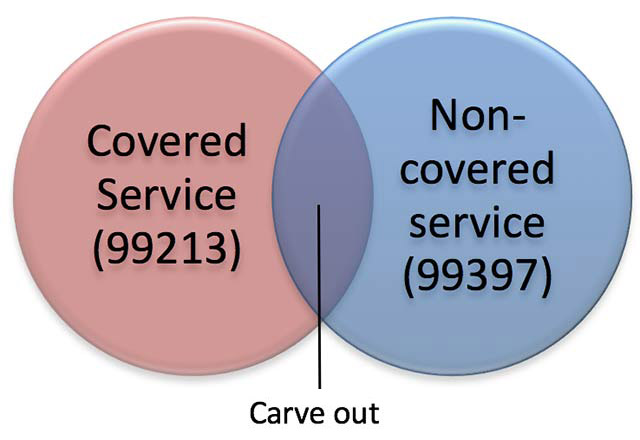
Medicare Cleave-out Services
It is important to code all services provided, even if you retrieve Medicare will not cover the services. Medicare has strict rules when billing for covered and non-covered services on the same appointment. This is often referred to equally the "carve-out rule." For instance, in the case of a medically-necessary visit on the same occasion as a preventive medicine visit, you may bill for the non-covered (carved-out) preventive visit, merely must subtract your charge for the covered service from your accuse for the not-covered service. For case, a problem-oriented visit allows for a history and examination, as does a preventive visit. The "carve out" eliminates the duplicate payment for these elements, paying you for performing the service only one time.
Patients demand to be enlightened of cost-sharing when a trouble-oriented visit is billed on the aforementioned occasion as a non-covered preventive visit. An ABN is not required, but a conversation with your patient earlier the services are rendered would exist appropriate.
For instance, a 67-year-old established patient presents for a covered service, such as an office visit for a chronic illness (e.g., 99213). At the aforementioned come across, the patient chooses to receive a preventive medicine examination (eastward.1000., 99397), which is a non-covered service under Medicare.
| SERVICE | Charge Corporeality |
|---|---|
| 99397- preventive exam (not-covered service) | $201.00 |
| 99213- office visit (covered service) | -$130.00 |
| Patient billable corporeality for 99397 | $71.00 |
Bundled Services
Medicare and most other payers do not allow for services to be "unbundled" when it has designated a prepare of services every bit represented past one payment (bundled). Examples include pre-operative and mail service-operative care when billing for a surgery or billing for multiple laboratory procedures when a single panel test represents the service performed. When Medicare or another payer designates a service equally "bundled," it does not make separate payment for the pieces of the bundled service and does not let you to pecker the patient for it since the payer considers payment to already be included in payment for another service that it does comprehend.
Coordination of Benefits
All payers will demand that correct coordination of benefits be followed for claims payment. Medical services are not always the responsibility of a wellness insurer. Payment may be the responsibleness of other entities, such as automobile insurance, workers' compensation, liability insurance, etc. Likewise, if a patient has multiple health insurance coverage (e.k., Medicare and employer coverage), one wellness insurer may be main, and the secondary insurer will not pay until the primary policy has paid. You should verify coordination of benefits in all cases of accident, injury, and when multiple insurance policies are involved.
Reference
Medicare Learning Network (https://www.cms.gov/Outreach-and-Educational activity/Medicare-Learning-Network-MLN/MLNProducts/Downloads/Items-and-Services-Not-Covered-Under-Medicare-Booklet-ICN906765.pdf)
Likewise in this Section
Billing For Services Not Provided To Medicare ?,
Source: https://www.aafp.org/family-physician/practice-and-career/getting-paid/coding/non-covered-services.html
Posted by: richardsonscance.blogspot.com


0 Response to "Billing For Services Not Provided To Medicare ?"
Post a Comment